Tuberous Breasts Surgery (Hypoplasia) Sydney
- Rebates from Private Health Insurance and Medicare
- Hospital fees covered by private health insurance
- Day surgery only
Tuberous breasts are a result of a congenital abnormality, and both men and women can be affected. The abnormality tends to start developing during puberty, and it may worsen with age. Tuberous breasts have several other names, such as constricted and conical-shaped breasts.
Signs of this condition include having enlarged areolas, a large gap between your breasts, a very high mammary fold (where the underwire of your bra sits), narrow breasts, minimal breast tissue, descending of the breasts, or different-sized and shaped breasts. It is also possible for tuberous breasts to affect the ability to breastfeed.
In general, tuberous breast correction surgery may involve a combination of techniques, including breast augmentation mammoplasty (implants) and/or a breast mastopexy (lift).
The outcomes shown are only relevant for this patient and do not necessarily reflect the results other patients may experience, as results may vary due to many factors, including the individual’s genetics and lifestyle.
What to expect during a tuberous breast consultation?
Dr Norris will take measurements of your breasts and explain what tuberous grade you are. You will then have a discussion with Dr Norris about your concerns and what you would like your breasts to look like after surgery.
Dr Norris will also evaluate your breasts by looking at your skin tone, the condition of the breast and fat tissue as well as the position of your nipples. He will measure your breasts, and photographs will be taken for your medical records. Next, Dr Norris will discuss how the operation is performed, where the incisions can be placed and what types of implants and sizes are available. You will then be given a detailed quotation, which will include the various options for tuberous breast surgery. If you decide to proceed with surgery, Dr Norris will see you again for a second consultation.
During your second consultation, your surgery will be scheduled, and Dr Norris will provide detailed instructions on preparing for the procedure.
What type of implant will be used?
There are a lot of decisions to be made when selecting an implant. Below is a beginner’s guide to understanding implants:
Surface
- Smooth
- Textured
- Polyurethane (furry Brazilian)
Profile
- Low
- Moderate
- High
- Extra High
- Ultra High
Shape
- Round
- Anatomical (teardrop):
- Oval Base Anatomical profile inferior lower pole
- Round Base Teardrop profile moderate lower pole
- Oval base Anatomical pole superior lower pole
And, of course, one of the other most important decisions is your implant size. There is currently no scientific evidence that silicone gel breast implants put you at an increased risk of breast cancer, autoimmune diseases or cause problems when breastfeeding. There is a small chance that these implants may interfere with the interpretation of a mammogram, but this can be avoided if special views are requested at the time of the scan. Evidence also suggests textured and polyurethane-coated implants help reduce the risk of scar tissue formation (capsular hardening) in the breast pocket around the implant.
Dr Norris will advise you if he thinks you may require two implants of different sizes. Most breasts are asymmetrical, but only a handful will require implants of different sizes. While most implants increase in 15-25cc increments, the majority of women are only 5-10cc different in size between breasts.
How tuberous breast surgery is performed?
Dr Norris only performs breast surgery in fully accredited medical facilities. Before the procedure, you will be introduced to the anaesthetist who works closely with Dr Norris. You will be taken through the final details of the procedure, and a general anaesthetic will be administered.
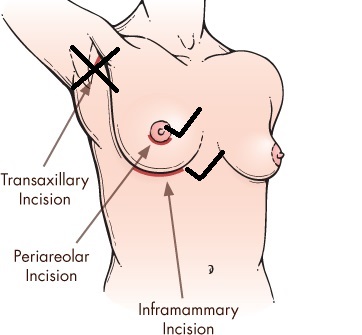
There are normally three incision placement choices, meaning any scarring will form accordingly. However, with tuberous conditions, you may only require one incision. In most instances, the incision is made around and through the areolar or under the breast in the mammary crease.
- Inframammary – (hidden in the fold under the breast)
- Periareolar – (hidden around the edge of the areola)
After Dr Norris has made the incision, the pocket in which the implant will be placed is dissected. This means that excess breast tissue and skin will be removed.
This pocket lies behind the natural breast tissue, on top of the chest wall muscle (subglandular) or either beneath the chest wall muscle (submuscular/subpectoral) .
The pocket that is used will depend on a number of factors, including the presence of breast ptosis and the type of implant used. Dr Norris most commonly places the implants in the submuscular position as it is easier to hide the implant and lessens the chances of the implant being felt. However, 50% of tuberous cases may need to have the implants placed on top of the muscle to address the tuberous shape of the breasts.
When the implant is placed in the pocket, it will be centred beneath the nipple and carefully positioned. Very occasionally, a drain may be placed in each pocket, but it will be removed the day after breast surgery. The incisions are then closed with dissolvable sutures. After the procedure, a waterproof dressing is applied over the incisions, and you will leave the hospital wearing a comfortable and supportive surgical bra.
What happens after the surgery?
- Breast surgery for tuberous breasts can take between 1-3 hours to perform depending on the incisions that will be used and how asymmetrical your breasts are.
- You will be hospitalised for approximately 5-7 hours before discharge.
- A friend or responsible adult must collect you from the hospital as you cannot drive home. Not only will your range of movement be restricted, but your pain medication might cause drowsiness.
- Dr Norris will send you home with detailed aftercare instructions as well as a prescription for pain medication.
- Daily short showers are permitted, provided your waterproof dressings are dried adequately.
- It’s highly recommended that you sleep on your back, elevated by a few pillows, for the first six weeks. Sleeping this way is more comfortable and will reduce swelling.
- Pain levels will be at their worst during the first two days after surgery, but this can be managed with pain medication.
- It’s common to experience bruising, swelling, tenderness, and sensitivity. Swelling can vary from patient to patient and should resolve within two weeks.
- Light exercise such as walking is permitted after one week. Your normal exercise routine can usually be resumed after six weeks, but Dr Norris will advise you accordingly.
- You can return to work after one week unless it involves heavy lifting or use of the upper body. You may need to stick to lighter duties for the first three weeks.
- A follow-up appointment will be booked for you on day three after the operation. This is to check your wounds and change the dressing./li>
Possible complications of tuberous breast surgery
- Rupture – Breast implants are not meant to last a lifetime. Breast implants can rupture when the shell develops a tear or hole. Ruptures can occur at any time after implantation, but they are more likely to occur the older the implant gets. Severe capsular hardening can also cause an implant to rupture.
- Capsular hardening – A hard capsule can form around the implant due to the body’s natural response to foreign material. Breasts that have capsular hardening will appear firmer and look different.
- Haematoma – Occurs when excess blood collects in one or both breast pockets. The blood is either absorbed naturally or will require surgical drainage. Symptoms include swelling, pain, bruising, skin that is hot to the touch, and itchy breasts.
- Infection – Infection can occur if microorganisms enter the incision sites. Any type of infection should be treated as soon as possible using antibiotics.
- Stretch marks – These are unpredictable and vary between patients. To prevent them, we advise using vitamin E and bio-oil before and after surgery to soften the skin.
How much does tuberous breast surgery cost in Sydney?
Tuberous breast surgery is a highly personalised procedure. No two patients will require the same approach, so costs can vary significantly. Scheduling a personalised consultation with Dr Norris is the best way to obtain a more accurate quotation as this will include your unique requirements and hospital and anaesthetist fees. Since tubular breasts are seen as a deformity, both Medicare and private health insurance providers will generally cover some of the costs associated with surgery. Dr Norris can provide more details on applying for a Medicare rebate during your first consultation.
Here at Form & Face, we provide patients with a
Lifetime followup guarantee
This means that we will be there for you far beyond the recovery period.
You can rest assured knowing that you can come to us about any
post-surgical concerns for the rest of your life.